The red imported fire ant (Solenopsis invicta), once native only to parts of South America1 and historically contained to the southeastern United States, is on the move. Rising temperatures, increased rainfall, and soil transport through landscaping and agriculture have allowed this aggressive species to expand far beyond its original range. For allergy specialists, this migration signals more than an ecological concern, it is an emerging medical threat that demands attention.
As fire ants spread into new territories, they bring potent venom with them capable of inducing severe allergic reactions in a population who has never encountered fire ants before. Allergists across the country must prepare for this shifting landscape by understanding the clinical risks and ensuring their patients are protected.
WARNING Important Safety Information (See full prescribing information for complete boxed warning.)
Intended for use only by licensed health care provider experienced in administering allergenic extracts and trained to provide immediate emergency treatment in the event of a life-threatening reaction. Observe patients for at least 30 minutes following administration. Immunotherapy may not be suitable for patients with medical conditions that reduce their ability to withstand a systemic reaction. Allergenic extracts can cause serious systemic reactions, including anaphylactic shock and in rare cases death, especially in patients who have severe or steroiddependent asthma, cardiovascular disease, or in patients who use beta blockers. Do not inject intravenously. This product is intended for subcutaneous injection for immunotherapy and percutaneous use for diagnosis. Refer to contraindications, warnings, precautions, adverse reaction and over dosage for more detailed information.
Fire Ant Expansion: Where Are They Going?
However, recent climate data and ecological studies show that fire ants are expanding northward and westward. Research from the USDA Agricultural Research Service estimates that fire ants could spread into larger portions of the Mid-Atlantic, the lower Midwest, the Southwest, and even parts of California, Arizona, and Oregon if warming trends continue.2
This means that areas previously considered safe from fire ant infestations are now seeing reports of colonies and stings.3 For allergists in these states, fire ant sensitization and anaphylaxis are becoming a new clinical reality.
Fire Ant Venom as a Potent Allergen
While most people experience localized pain, swelling, pustule formation, a significant subset may develop systemic reactions. These reactions range from generalized hives and angioedema to full-blown anaphylaxis with hypotension, airway compromise, and cardiovascular collapse.
Studies show that up to 20% of fire ant stings result in large local reactions, and approximately 0.5% – 2% of stung individuals may experience systemic allergic reactions. In highly colonized regions, 8.5% – 51% of residents may be stung each year, putting a sizable population at risk.5
The Clinical Impact of Fire Ant Allergies
With fire ants spreading to new states, allergists must now consider fire ant allergy in patients presenting with systemic reactions to insect stings in general, especially in areas where fire ants were previously non-endemic.
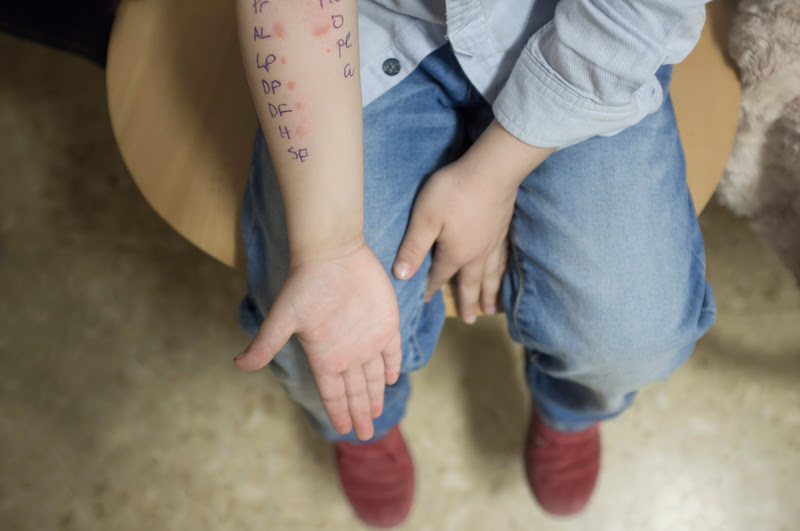
Diagnosis
- Skin testing for Solenopsis invicta venom is a primary tool for diagnosing fire ant allergies.
- Skin testing results in the most specific diagnosis of fire ant allergies by utilizing IgE detection.6
Risk Stratification
- Patients with prior systemic reactions, outdoor workers, children, and the elderly are at risk of severe reactions to fire ant venom.
- Those with multiple exposures such as landscapers, gardeners, and construction workers may become sensitized over time.
Patient Education
- Patients should be taught how to recognize the signs of anaphylaxis and learn their options for treatment, such as allergy immunotherapy.
- Avoidance strategies should be emphasized, especially in newly infested regions.

Immunotherapy for Fire Ant Allergies
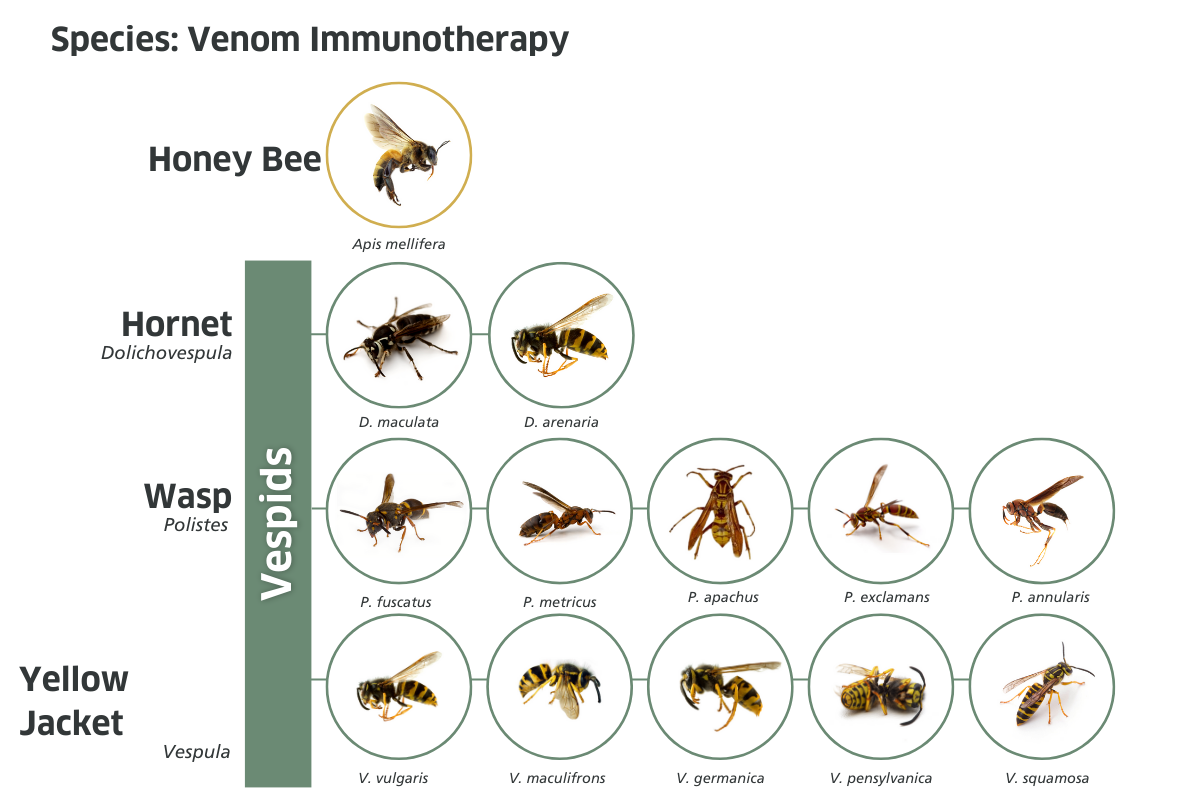
Allergy immunotherapy for fire ant venom is highly effective in preventing systemic reactions at a similar rate to venom immunotherapy for flying Hymenoptera venom.7
Key Facts
- Fire ant VIT uses whole-body extract of Solenopsis invicta to produce the extract.
- The standards course includes build-up injections followed by maintenance injections typically given every 4 weeks.
- Patients often remain in the maintenance phase of immunotherapy for 3 to 5 years.
- Even though skin test often remain positive, clinical protection is maintained long after desensitization.7
Why Trust HollisterStier Allergy?
When it comes to venom immunotherapy, product quality and reliability matter. HollisterStier Allergy is a leading US manufacturer of FDA-approved allergenic extracts, including those used for fire ant venom immunotherapy.
Why Choose HS Allergy?
- High-quality extracts manufactured to rigorous standards for purity and potency.
- Consitency and reliability ensures each vial provides reproducible clinical performance.
- Responsive customer support with a dedicated team that understands the needs of allergists.
- Secure supply chain where we harvest and produce our extracts in house, minimizing disruptions, even during periods of increased demand.
As fire ant migration introduces venom allergy risk to new patient populations, having a dependable source of fire ant extract is crucial. Protect your patients with HollisterStier Allergy, no matter where fire ants move next.
Prepare Your Practice for Fire Ants
As ecological patterns change and insect species migrate, allergists must adapt. Fire ant allergies are no longer region specific, the clinical burden is shifting to allergists in new states and regions and will continue to do so as climate change progresses.
Here’s what you can do to best support your patients:
- Stay informed by monitoring entomological data and reports of fire ant spread in your region.
- Educate your team by training staff to recognize symptoms and risk factors for fire ant allergy.
- Stock the right extracts by ordering Solenopsis invicta venom immunotherapy from a trusted source like HollisterStier Allergy.
- Engage with your community and raise awareness with patients within your community about the rising risks of fire ant allergies.
The expansion of fire ants across the US is no longer a hypothetical, it’s happening now. With that expansion comes increased allergic risk, more anaphylactic events, and a need for proactive treatment planning.
Allergists must lead the response. By diagnosing early, educating patients, and administering effective immunotherapy using reliable extracts, we can dramatically reduce the burden of fire ant venom allergy.
Article References
- “Red Imported Fire Ant.” Center for Invasive Species Research, cisr.ucr.edu/invasive-species/red-imported-fire-ant.
- “Potential United States Range Expansion of the Invasive Fire Ant : USDA ARS.” gov, 2017, www.ars.usda.gov/southeast-area/gainesville-fl/cmave/imported-fire-ant-and-household-insects-research/docs/potential-united-states-range-expansion-of-the-invasive-fire-ant/.
- “Antmaps.org.” org, 2020, antmaps.org/?
- Zamith-Miranda, Daniel, et al. “The Allergic Response Mediated by Fire Ant Venom Proteins.” Scientific Reports, vol. 8, no. 1, 26 Sept. 2018, p. 14427, www.nature.com/articles/s41598-018-32327-z, https://doi.org/10.1038/s41598-018-32327-z. Accessed 29 Sept. 2023.
- Lopez, Diego J., et al. “The Human Health Impacts of the Red Imported Fire Ant in the Western Pacific Region Context: A Narrative Review.” Tropical Medicine and Infectious Disease, vol. 9, no. 4, 1 Apr. 2024, p. 69, www.mdpi.com/2414-6366/9/4/69#:~:text=Around%2025%25%20of%20those%20stung, https://doi.org/10.3390/tropicalmed9040069.
- Kruse, Brian, et al. “Fire Ant Bites.” PubMed, StatPearls Publishing, 2021, www.ncbi.nlm.nih.gov/books/NBK470576/.
- Neaves, Brittanie I, and Christopher A Coop. “Imported Fire Ant Immunotherapy.” Annals of Allergy Asthma & Immunology, vol. 133, no. 1, 26 Jan. 2024, pp. 28–32, https://doi.org/10.1016/j.anai.2024.01.014.